A key challenge for malaria elimination is the identification of individuals in malaria-endemic communities who, often without symptoms, serve as a reservoir of malaria infection. Typically, information about the human reservoir of malaria infection comes from tests that detect the parasite directly (such as microscopy, rapid diagnostic test, and polyermase chain reaction assays). While informative, these approaches are limited by the fact that they sample ‘a moment in time’ and fail to capture information on each individual’s exposure history. Malaria serology, which tests for antibodies to parasite antigens, provides information on exposure history. However, traditional approaches to serology, such as ELISA, test for a single antigen at a time, are laborious and generally limited to assessment of several antigens.
Plasmodium has enormous genetic diversity and a complex life cycle which together result in an extensive number of possible antigen targets in the infected human. At present, it is not clear which antigens are the best markers of prior malaria exposure under various conditions of exposure.
In her presentation at this year’s ASTMH, Dr. Andrea Berry explained how researchers at the University of Maryland’s Division of Malaria Research have employed microarray technology as a tool to identify key serological markers of malaria exposure, offering the potential to radically improve our ability to assess human reservoirs of malaria transmission. While protein microarrays can assess several hundred antigens in a single run, the Maryland team, working with Roche Madison, has developed a peptide microarray assay which is even more powerful. This assay can quantify antibody responses to over 170,000 peptides, where each peptide represents a segment of a whole protein. The microarray includes 42 proteins, each with a large number of variants. The proteins represented by this chip were selected based on their potential as vaccine targets or as markers of malaria exposure (including malaria gametocytes antigens, variant surface antigens and mosquito salivary antigens).
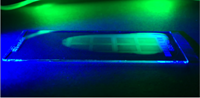
While microarray technology is highly complex, the data it produces is surprisingly accessible. The microarray chip is a matrix, where each ‘tile’ represents a unique peptide. Antibodies bind to the corresponding peptides on the microarray and are detected by a fluorescent marker; the more antibodies bind to a peptide, the greater the florescence. The strength of each person’s antibody reactivity to each peptide, and thus each protein, is quantified based on florescence. Beyond protein-specific responses, microarray data reveal another important aspect of an individual’s serological profile, the breadth of their antibody response, as shown in the number of variants of each antigen to which their antibodies react. Wider breadth of response and stronger reactivity are both indicators of greater malaria exposure, and thus increased potential to serve as a reservoir of infection. To understand malaria exposure on a community level, microarray data from field studies can be analysed in a number of ways, for example by showing the average response rates to a specific antigen by age or other demographic characteristics.
Given the enormous number of potential antigen targets involved in malaria infection, an important goal of the Maryland team’s work is to identify specific antigens that can distinguish between low and high exposure groups. In data from Bandiagara, Malawi, the team’s preliminary analysis has identified 86 peptides that were significantly more reactive in adults (a highly exposed group in this endemic setting) than in children. The team intends to carry out further studies to refine the peptide microarray and increase our understanding of key serological markers of malaria exposure with the goal of identifying peptides that may be used as a point of contact surveillance tool. For further information on the team’s work, please contact Dr. Andrea Berry (
[email protected]).
This blog was written by Ingrid Peterson, University of Maryland.